Bladder Control Problems
Is Your Bladder in Control? Take Charge
Gotta go, can’t go or go when you don’t want to go? Our comprehensive urogynecology practice helps you take back control of your bladder, offering every treatment available for a broad range of bladder control problems.
We start with:
- A detailed physical exam that looks at the basic function of your pelvic floor muscles and your bladder
- A urinalysis or urine test to check for infection
- Urodynamic testing: This hour-long test checks the bladder’s ability to hold and release urine steadily and completely.
- Cystoscopy: During this 15-minute exam, a urogynecologist uses a special telescope to look inside your bladder and urethra, the tube that carries urine from the bladder to the outside of the body.
Based on these results, we can diagnose your problem and offer the treatment that is best for you.
Overactive Bladder
Are you part of the overactive bladder club? You could be if you experience these symptoms:
- Urgency: Gotta go now
- Urge incontinence: Gotta go now, with leakage
- Frequency: Gotta go often
- Nocturia: Gotta go all night long
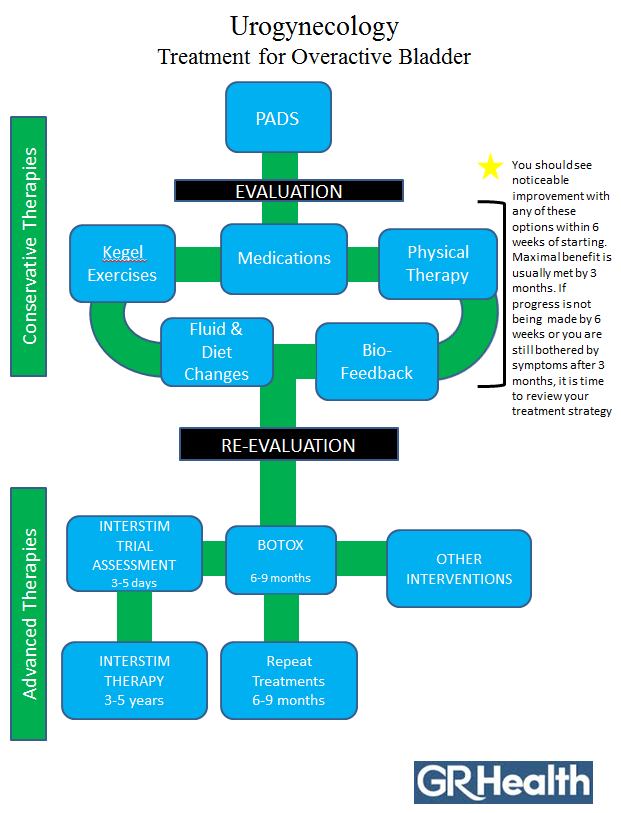
These feelings happen when your bladder muscles squeeze to empty out urine even when your bladder isn’t full (a full bladder holds about two cupfuls). Your urogynecologist may suggest one or a combination of treatments, including:
- Lifestyle changes: Including using pads, making diet changes and training yourself to go only when you really need to go. A bladder diary can be helpful in tracking frequency.
- Physical therapy: Pelvic floor exercises, including Kegel exercises, can retrain and strengthen your bladder muscles. Used in conjunction with exercise, biofeedback can help you pinpoint and better control these muscles.
- Medications: Including bladder muscle relaxants
- Botox injections: When injected into the bladder wall muscles, Botox can effectively relax these muscles for several months, reducing inappropriate urges to go and allowing your bladder to hold more urine
- Percutaneous tibial nerve stimulation (PTNS): A form of neuromodulation therapy, PTNS is 12-week series of 30-minute treatments that deliver a mild electronic stimulation to the nerves that control bladder function.
- InterStim: This neuromodulation device is implanted in the body and sends gentle electronic pulses to the nerves that control bladder function, helping to regulate them.
Urinary Retention
Urinary retention is an uncomfortable condition where you may feel an urgent need to urinate, but simply can’t. You may have trouble starting, have a weak stream or feel as though you still need to go even though you’ve just gone. Because you can’t empty your bladder completely, this leads to discomfort or pain, bloating and infection.
If you’re not able to urinate at all, this is an emergency condition and you should seek help right away.
Urinary retention most commonly affects those in their 70s and 80s and may be caused by:
- Obstruction (blockage) of the urethra, the tube that carries urine out of the body
- Medications
- Nerve problems or weakened bladder muscles
We offer the following treatments and care for patients suffering from urinary retention:
- Catheter management. Patient suffering from chronic urinary retention may require one-time, regular or ongoing catheter management to help release urine.
- Treatment of obstructions, including correcting blockages caused by prolapse, slings or other procedures.
- InterStim. This neuromodulation device is implanted in the body and sends gentle electronic pulses to the nerves that control bladder function, helping to regulate them.
Stress Incontinence (Leaky Bladder)
Coughing. Sneezing. Laughing. Exercise. These common activities can all trigger a urine leak if you suffer from stress incontinence.
Stress incontinence happens when there are problems with the muscles or nerves that help to hold or release urine. Our urogynecology practice offers a wide range of conservative and surgical procedures that can help stop frustrating bladder leaks, including:
- Physical therapy: Pelvic floor exercises, including Kegel exercises, can help strengthen your bladder muscles.
- Pessaries, rubber rings similar to the outer ring of a diaphragm: When inserted into the vagina, pessaries can help control incontinence.
- Bulking therapy: During this in-office or outpatient procedure, your urogynecologist injects a safe gel-like material around the urethra, the tube that carries urine out of your body. The gel bulks up the area to help block leakages.
- Surgery: A surgically implanted sling or permanent sutures support the urethra. Up to 90 percent of women undergoing these procedures experience improvement or cure. Learn more about mid-urethral slings by downloading this FAQ from the American Urogynecologic Society and the Society of Urodynamics, Female Pelvic Medicine & Urogenital Reconstruction.
Other Conditions
Our experienced urogynecology practice also treats many other bladder control conditions, including:
- Mixed incontinence, such as a combination of stress incontinence (leaky bladder) and overactive bladder
- Unpredictable incontinence
- Fistulas, holes in the bladder wall that cause leakages into the vagina
Patient Education
Download these information guides offered by the International Urogynecological Association for more answers to your questions.
- Overactive Bladder
- Botox for Overactive Bladder
- Leaky Bladder/Stress Urinary Incontinence
- Urethral Bulking for Stress Urinary Incontinence
- Bladder Training
- Bladder Diary Form
- Cystoscopy to Diagnose Bladder Control Problems
Schedule an Appointment Now
To make an appointment, call us at 706-446-1300. Our friendly specialists will schedule a time as soon as possible.
Or leave a message on our Consult-a-Nurse line. Our practiced urogynecological nurses will respond to your question within 48 hours. Call 706-721-6741.